After 37 years of pioneering health journalism, community engagement, and empowerment through information, we have now ceased operations.
This website will be accessible until September 2025, with all the information being up to date as of July 2024.
If you are a supplier, or another partner you can contact our legacy email address as [email protected] with any queries.
We extend our heartfelt thanks to everyone who supported our vision for a world where HIV is no longer a threat to health or happiness. Together we have made a difference.
With Gift Aid, your generous donation of £ 10 would be worth £ 12.50 at no extra cost to you.
I am a UK taxpayer and I understand that if I pay less Income and /or Capital Gains Tax than the amount of Gift Aid claimed on all my donations in the relevant tax year, it is my responsibility to pay any difference.
In our 35th year we’re asking people to donate £35 – that’s just £1 for every year we’ve been providing life-changing information. Any donation you make helps us continue our work towards a world where HIV is no longer a threat to health or happiness.
- £5 allows us to reach millions of people globally with accurate and reliable resources about HIV prevention and treatment.
- £10 helps us produce news and bulletins on the latest developments in HIV for healthcare staff around the world.
- £35 means we can empower more people living with HIV to challenge stigma with our information workshops, videos and broadcasts.

Travel restrictions for people with HIV

- A number of countries restrict the entry and/or residence of people with HIV.
- Tourism or business trips are generally possible, even in countries with entry bans.
- Long-term restrictions related to work or study permits are strictly enforced.
- Undetectability is never taken into account.
Some countries limit entry for people with HIV. However, the number of countries restricting travel by people with HIV has reduced in recent years. Short-term trips usually have fewer restrictions and checks may be less consistently carried out. The rules tend to be more strictly enforced for longer-term stays, such as those requiring a work visa.
Can I travel if I am living with HIV?
Yes. Many countries clearly state that your HIV status will not affect whether you can visit, stay, or work. Most countries do not require any type of medical tests for short-term or long-term stays.
However, there are still some countries which do limit entry for people living with HIV. A small number of these have an entry ban. This means that if you travel to these countries and you are living with HIV, you might not be allowed to enter.
In other countries, restrictions only apply to longer stays. You might be allowed to enter for a short time (such as for a holiday), but not be allowed to work or live there. In these countries, you may have to take an HIV test or declare your HIV status when applying for a visa or residency permit. In some cases, you might not be asked for information about HIV, but if you are found to have HIV you could be deported (made to leave).
Travel restrictions for people living with HIV are complex and they change from country to country. Not all countries have specific immigration laws relating to HIV, but declaring your HIV status can still sometimes cause issues.
Travel restrictions apply even if you have an undetectable viral load.
Which countries have HIV travel restrictions?
This page has general guidance on current regulations across different continents, based on information from the website www.hivtravel.org . This is provided by Deutsche AIDS-Hilfe, the European AIDS Treatment Group and the International AIDS Society.
Please note that the regulations may have changed since the time of writing. Before you make any travel plans, including to live or work abroad, we recommend you check the www.hivtravel.org website for up-to-date details by country. There is also a feedback form for those who need additional advice or have information to improve the site.
North America
For entry and short-term stays, there are generally no restrictions for people living with HIV travelling to North America.
In the US, people entering with prescription medication, including HIV medication , need to carry a doctor’s certificate in English, stating that the drugs are required to treat a personal condition.

Find out more: Travelling with HIV medication
In Canada, you have to take an HIV test if you plan to stay for more than six months. All long-term visitors are assessed in terms of how much ‘excessive demand’ they might put on the Canadian health service. A cost of more than CA$24,057 a year is considered ‘excessive’, but the cost of many publicly funded HIV medications is less than this amount.
Central and South America
For entry and short-term stays, there are generally no restrictions for people living with HIV travelling to Central and South America.
There are restrictions on long-term stays in Honduras, Nicaragua, and Paraguay. In Paraguay, for example, those travelling to the country because they want to apply for permanent residency have to take an HIV test. A residence permit won’t be granted if the test is positive, unless you can pay for your treatment yourself.
For Aruba, Belize, Nicaragua, and Suriname, the regulations are unclear or inconclusive. Contact their respective embassies for guidance before travelling.
For entry and short-term stays, there are generally no restrictions for people living with HIV travelling to the Caribbean.
Cuba, the Dominican Republic, St Vincent and the Grenadines, Turks and Caicos, and the Virgin Islands all have restrictions on long-term stays. For example, in St Vincent and the Grenadines, work permits are not renewed in the case of a positive HIV test result and HIV-positive foreigners have no access to treatment and services.
In the Cayman Islands, Montserrat, St Kitts and Nevis and St Vincent and the Grenadines, regulations are unclear or inconclusive. No information is available for Bermuda. Contact their respective embassies for guidance before travelling.
Sub-Saharan Africa
There are generally few restrictions for people living with HIV travelling to sub-Saharan Africa. However, in Equatorial Guinea, you may have to present an HIV test certificate. If you are HIV positive you might be refused entry or deported.
The following countries have restrictions on long-term stays: Equatorial Guinea, Mauritius, Seychelles, and Sudan.
Regulations are unclear or inconclusive in Angola and there is no information available for São Tomé and Prinicipe. Contact their respective embassies for guidance before travelling.
North Africa and the Middle East
Most of the countries that restrict entry based on HIV status are in North Africa and the Middle East.
Living with HIV may mean you are not allowed to enter Jordan, Iran, Iraq, the United Arab Emirates, or Yemen, even for a short stay. However, there are no restrictions if you’re passing through Dubai in transit as an airline passenger.
Countries with restrictions, or potential restrictions, on long-term stays include Algeria, Bahrain, Egypt, Israel, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, Syria, and Tunisia. Almost all these countries will also deport people based on their HIV status.
Note that regulations are unclear or inconclusive in Iran, Qatar, and Tunisia. You are advised to contact their respective embassies for guidance before travelling.
Western, northern and southern Europe
For entry and short-term stays, there are generally no restrictions for people living with HIV travelling to western, northern, or southern Europe.
In Cyprus, people from outside the EU who are applying for a temporary residence permit have to prove they don’t have HIV before a permit will be issued. However, this rule doesn't apply to diplomatic personnel and high-ranking company employees.
Central and eastern Europe
In Russia, no HIV testing is required for short-term tourist stays (up to three months), but foreign residents found to be HIV positive are expelled. You are required to present a negative HIV test result for a stay longer than three months, or if you are using a multi-entry visa.
"Travel restrictions for people living with HIV are complex and they change from country to country."
In Bosnia and Azerbaijan, there are restrictions on long-term stays, and in Slovakia, people from outside the EU applying for a temporary residence permit have to prove they don’t have HIV before one is issued.
In Hungary, you have to report your HIV status when applying for a residence permit. However, being HIV positive can’t be used as a reason for denying your permit application.
Central Asia
Kazakhstan, Kyrgyzstan, and Uzbekistan all have restrictions on long-term visits, but the rules are unclear or inconclusive. Contact their respective embassies for guidance before travelling.
For entry and short-term stays, there are generally no restrictions for people living with HIV travelling to east Asia.
China used to ban short-term visitors with HIV, but it doesn’t anymore. However, the website www.hivtravel.org recommends that you don’t declare your status on visa application forms. It also advises that you should be careful with voluntary status declarations, such as wearing red ribbons. An HIV test is required for work and study visa applications of more than six months. However, Hong Kong and Macau have separate entry and visa regulations without any restrictions.
The only country in east Asia that deports people because of their HIV status is the Democratic People's Republic of Korea (North Korea).
South and south-east Asia
There are generally few restrictions on entry and short-term stays for people living with HIV travelling to south and south-east Asia.
However, people living with HIV are not allowed to enter Brunei and people who are found to be HIV positive can be deported. In Bhutan, you have to present the results of an HIV test that was taken in the six months before your visit if you want to stay longer than two weeks. People who test positive may be deported.
In the Maldives, Malaysia, and Singapore there are restrictions on longer-term stays.
The regulations in Malaysia and Sri Lanka are unclear or inconclusive. Contact their respective embassies prior to travelling for guidance.
For entry and short-term stays, there are generally no restrictions for people living with HIV travelling to Oceania. The exceptions to this are the Solomon Islands, where entry may be denied on the basis of HIV status, and the Marshall Islands, where HIV testing is required for temporary visitors staying more than 30 days.
In Australia, all long-term visa applicants over the age of 15 have to take an HIV test. For those under 15, an HIV test might also be carried out if you have a history of blood transfusions, your mother is living with HIV, or there is a medical sign that you might be living with HIV.
Long-term visa applicants who have any long-term health condition, including HIV, are considered according to how much they might cost the Australian health system. Information on this can be found on the Australian government’s website.
In New Zealand, people with HIV are assessed on a ‘case by case’ basis. If you are living with HIV and in a ‘long-term stable relationship’ with a New Zealand citizen, you will be granted an automatic medical waiver. This means your HIV status isn’t considered as part of your application for a visa or residency permit.
The following countries also have restrictions on long-term stays: Marshall Islands, Papua New Guinea, Samoa, and the Solomon Islands.
In the Solomon Islands and Tonga, the regulations are unclear or inconclusive. For French Polynesia and Kiribati there is no information available on travel restrictions relating to HIV status. Contact their respective embassies for guidance before travelling.
Can I travel into a country with entry restrictions?
If you’re living with HIV and you decide to travel to a country that does have entry restrictions you may be refused entry or deported. Some countries will offer waivers that let you visit in certain circumstances, such as if the trip is to visit family members, but they can be difficult to get.
Travel restrictions for people with HIV can change quickly and so they need to be checked before any trip. In countries where restrictions have been recently changed, you should take extra caution discussing your HIV status.
If you’re living with HIV you might have travelled into a country when a travel ban was in place. In this case, it’s important to know that there is still a risk of being deported even if the travel ban has now been lifted. This could happen if there was proof you knew your HIV status and still entered the country. In this case, you could be deported for breaking the law.
Can I travel with PrEP medication?
We are not aware of any countries that ban people who are travelling with PrEP. However, most countries limit the amount of prescription medication you can travel with. Usually, you will be able to take enough medication for up to a three-month stay. But should always check the rules for the countries you are travelling to and from, as some have stricter rules. It’s usually a good idea to bring your prescription with you .
If a country has entry restrictions for people with HIV, travelling with PrEP might cause problems. This is because customs officials might think the medication is for treating HIV. In extreme cases, it could even mean you are deported (made to leave the country). A letter from your doctor explaining PrEP is for HIV prevention might help.
Other useful information
When you contact an embassy or consulate to ask about travel restrictions, you can keep your name or HIV status anonymous. For British Overseas Territories, the Foreign, Commonwealth & Development Office website is a good place to start.
It may be helpful to contact an HIV organisation in the country you are travelling to and ask them for information.
There is more information about accessing HIV services and medication in some European and central Asian countries on the Stay on ART website.
You might also find the following pages useful:
- Travelling with HIV medication
- Travel insurance for people with HIV
- HIV and travel
- HIV criminalisation laws around the world

United States of America - Regulations on Entry, Stay and Residence for PLHIV
Restriction category relative to united states of america.
- Countries without restrictions
HIV-specific entry and residence regulations for United States of America
U.S. President Barack Obama has announced that all current restrictions affecting people with HIV from entering or migrating to the United States are lifted as of January 4, 2010. Since January 4, 2010, people living with HIV can enter the U.S. like anybody else.
Visitors under the visa waiver program (for countries where a visa is not required to travel to the USA) and are living with HIV: please note that HIV is no longer considered a communicable disease for entry purposes. When submitting the online ESTA form to clear your entry to the U.S., it is important that you do check „no“ for the question about communicable diseases. HIV is no longer considered as such by the U.S. authorities.
Customs regulations require people entering with prescription medication like antiretroviral drugs to carry a doctor’s certificate in English, stating that the drugs are required to treat a personal condition. This requirement is strictly enforced by U.S. customs authorities and it applies to all prescription drugs.
(Sources: 1, 2, 4)
A citizen of a foreign country who wishes to enter the United States must first obtain a visa, either a non-immigrant visa for temporary stay, or an immigrant visa for permanent residence. Similarly, a student visa (F or M) is required to study in the U.S. Foreign nationals may not study after entering on a visitor (B) visa or through the Visa Waiver Program (VWP), except to undertake recreational study (non-credit) as part of a tourist visit.
A 2009 rule by the U.S. Centers for Disease Control and Prevention established that HIV infection is no longer defined as a communicable disease of public health significance and testing for HIV infection is no longer required as part of the U.S. immigration medical screening process. Additionally, HIV infection no longer requires a waiver for entry into the United States.
Since HIV is no longer defined as a communicable disease of public health significance, international students should not worry about traveling with their antiretroviral (ARV) medications. Students are encouraged to arrive in the U.S. with at least three months of ARV medications, in their original bottles for easy identification.
Author’s note: U.S. customs regulations require everybody to carry a doctor’s prescription for all prescription medication.
There is no national health care coverage in the United States. The U.S. Department of State requires exchange visitors on a J (exchange visitor) and their dependents be covered by medical insurance for the length of their program. While the State Department has no specific insurance requirements for international students and their dependents on an F visa, many universities require all international students to purchase health insurance. Visiting students living with HIV are encouraged to evaluate health insurance options for coverage of HIV medical services, notably antiretroviral medications.
Visiting students with HIV experiencing any problems, including anticipated medication shortages, should contact a community-based organization in the state they are temporarily residing. Some safety net programs are available to assist people with HIV with non-immigrant status (including F, M, and J visas), depending on their income and other criteria.
(Source: 5)
HIV treatment information for United States of America
Emergency rooms cannot turn away any patient in need of care, so people with HIV can go there. They will however be billed for the entire amount, which could be huge. Regular care will also be self-pay, unfortunately. Unless the patient’s country of residence has a mechanism for paying for out of country care, or they have travel insurance, it will be out of pocket.
(Source: 3)
HIV information / HIV NGOs in United States of America
Author’s note:
Use a web search engine to find local HIV organisations State by State .
- NASTAD Web: nastad.org
Global Criminalisation of HIV Transmission Scan
- Dr. Nancy Ordover and the authors, November 2, 2009, April 7 and 13, 2010
- Memorandum, U.S. Department of Homeland Security, U.S. Citizenship and Immigration Services, November 24, 2009
- Jeff Taylor, AIDS Treatment Activists Coalition, via e-mail, January 5, 2010
- Site authors, March 31, 2022
- Tim Horn, Director Health Care Access at NASTAD, via e-mail, March 31, 2022
updated: 3/31/2022 Corrections and additions welcome. Please use the contact us form.
Comments on HIV-restrictions in United States of America

User account menu
- Get connected
Immigration to the US, Women, and HIV: Facts and Resources

Lea esta hoja informativa en español
Table of Contents
The us immigration system, history of us immigration, health, and hiv, getting hiv care or prevention, women and us immigration, at the us border, where immigrants may find support.
Note: This fact sheet is intended for people who plan to stay in the US for longer than a visit. The information below is current as of the date on this fact sheet. However, immigration laws and their enforcement change rapidly, so some information here may no longer apply by the time you read this. This fact sheet is intended for information only and does not constitute legal advice. The Resources section lists organizations that may be able to provide legal help for your specific case.
The United States represents about 5 percent of the world's total population, yet is home to close to 20 percent of its migrants. There are more foreign-born people living in the US than in any other country in the world. This group makes up more than 13 percent of the US population and includes:
- naturalized citizens (people who have become citizens through a process other than birth)
- lawful permanent residents (green card holders)
- people who have sought asylum
- people on certain temporary visas
- people who are living in the country without required documents
If you are living with HIV, there is no legal barrier based on your HIV status to your making your home in the US. The rule restricting travel or immigration to the US by people living with HIV, often called the "HIV entry ban," was lifted in 2010 after 22 years by then-President Barack Obama.
View our companion fact sheet, US Immigration and HIV: The Basics , for an overview of the US Immigration system
From the early days of – generally European -- immigration to the US, the government has put regulations in place to try to keep out people with medical problems. In the late 1800s and early 1900s, when most immigrants passed through Ellis Island in New York City, doctors examined everyone who arrived and refused entry to those deemed too ill. The stated purpose was to keep communicable diseases out. We saw a similar process unfold as authorities around the world tried to stop a virus – COVID-19 – from spreading by closing national borders to people from other countries.
In the US, formal regulations that kept people from entering the country based on specific medical conditions were enacted in 1952. In addition to a list of specific illnesses, they included the catch-all phrase "any dangerous contagious disease." That wording was later changed, but the essential meaning remained. In 1987, AIDS was added to that list of conditions, and shortly thereafter also HIV. For the next 22 years, anyone living with HIV who was not a US citizen could be denied entry into the US based on HIV status alone. That ban was finally lifted in 2010. However, HIV status may still be used to discriminate against immigrants (see "At the US Border" below).
One of the major issues people living with HIV face in the US is the need for health insurance. Despite the passage of the Affordable Care Act (ACA or "Obamacare"), many people in low-wage jobs do not have affordable health insurance. Such jobs are often held by those new to the country. People who are in the US without proper documents are not eligible for any federally funded healthcare coverage, which includes the ACA marketplaces as well as Medicaid. Without health insurance, many people find it difficult to get HIV care and treatment. Services funded through the Ryan White HIV/AIDS Program supply that care to those without other insurance and may do so independent of immigration status.
Access to HIV-related care varies widely in the US. People get their care and services in a wide range of settings.
The "public charge rule" allows immigration officials to deny permanent residency in the US to people based on whether they have used public benefits in the past or are likely to use them in the future. The public charge rule, like regulations restricting entry by people with communicable diseases, dates back to the earliest federal immigration legislation. An immigrant's health status and access to private health insurance, among other issues, are considered when deciding whether to allow them to remain in the US indefinitely (get a "green card" without restrictions). However, relying on a Ryan White-funded clinic or the AIDS Drug Assistance Program (ADAP) for care and treatment would not be included as part of a public charge determination.
HIV status could also be used as a reason for applying for asylum, if the person can show that they face a credible fear of persecution because of their HIV status. However, the US has been limiting applications for asylum. These cases are also very challenging, require an attorney, and involve many obstacles (such as having to apply within one year of arriving in the US).
It is your right to ask about HIV-related care. If you are new to the US, or newly seeking HIV services, you may be wondering where you can get HIV treatment or learn more about HIV prevention depending on your immigration status.
Access to HIV-related care varies widely in the US. People get their care and services in a wide range of settings, and it is difficult to determine where to begin in a given area. Below is a list of places to start in your search for HIV-related services.
- An HIV/AIDS service organization in your area may provide valuable support, including helping you find HIV care or prevention (or providing care services themselves). POZ Magazine maintains a searchable directory of HIV and health services throughout the US and other parts of the world.
- Your local Ryan White HIV/AIDS Program provider. As discussed above, Ryan White-funded programs serve people living with HIV who may not be able to get medical care through other sources. You can use this tool to search for Ryan White services in your area.
- Regional public health offices. All US states and territories have departments of public health, though they go by different names in different areas of the country. Cities or counties may have their own public health departments within states as well. Health department staff members ought to be able to point clients in the right direction to access HIV care. Here is a list of state and territorial health departments from the US Centers for Disease Control and Prevention (CDC); the National Association of County and City Health Officials (NACCHO) also maintains a searchable list of local health departments .
- County hospitals are another central location where people can seek information about health services offered at that hospital, or referrals to other locations for care.
- Faith-based support. While not every religious institution is aware or openly welcoming of people living with HIV, many people may feel most comfortable seeking care through recommendations from members of their faith community. Many houses of worship even have HIV or health ministries dedicated to keeping their communities healthy.
- Looking for services to help you or your partner(s) remain HIV-negative? This article from PrEP Daily describes different resources and ways to access pre-exposure prophylaxis (PrEP) , a drug you can take regularly to prevent HIV. PleasePrEPMe.org is another great resource for finding PrEP services. The other locations detailed earlier in the list may also have information about PrEP and other forms of HIV prevention.
In recent years, it has become harder to claim asylum in the US on the grounds of experiencing intimate partner or gang violence in one's country of origin. Many Central American and other women are fleeing just such violence. They may also experience rape and sexual assault during their journey to the US. Beyond the psychological scars these experiences may leave, they also render the women highly vulnerable to acquiring HIV and/or other sexually transmitted infections (STIs) .
Anyone living with HIV who was not a US citizen could be denied entry into the US based on HIV status alone. That ban was finally lifted in 2010.
If a woman is assaulted within the US – sexually or otherwise – she may have the option of filing for a "U visa." This type of visa allows victims of certain "qualifying" crimes to petition to stay in the US to help the government investigate their assailants.
A U visa is available to people who are in the US without valid documentation, have become the victim of a serious crime, and are helping – or likely will help in the future – US authorities to solve the crime. Such help must be certified by a US police department or similar agency.
However, only a limited number of U visas is issued each year, and there is no guarantee that a person who applies for a U visa will receive one. At the time of this writing, there was a backlog of hundreds of thousands of people waiting to have their U visa applications reviewed, and the wait can be more than 10 years. Further, some who have gone through the process report that, when cases are reviewed, having to relive and explain violent crimes during assessments can be traumatic without appropriate mental health support.
Women are often also responsible for children. School-age children are required to be in school, regardless of their immigration status. Schools are "protected areas" under ICE's own policy. That policy also includes healthcare facilities, places of worship, and certain events, such as weddings or funerals. ICE is not supposed to arrest people for immigration violations in these places, except under specific circumstances. However, ICE has arrested people just outside these locations (e.g., parents on their way to pick up their children from school).
In early 2018, the US began to separate children from their parents when they entered the US from Mexico without proper immigration documents. The children were housed in group facilities -- some of which were converted warehouses -- with little or no care. Some children were handed over to foster parents who had not been screened for their ability to care for children.
Once the policy became known, many people organized to stop it, and in June 2018 the US government ordered ICE to stop separating families at the border in most cases. However, children can still be separated from their parents if the parent faces criminal charges – which could be something as minor as driving without a license during a previous stay in the US without proper documentation.
After parents and children who had been separated at the border were reunited, they were often allowed to live in the community while waiting for their asylum case to be filed and processed. This let them stay temporarily in the US "under color of law," but did not provide them with identification papers, a work permit, health insurance, or any other benefits. Various organizations and individuals helped out.
HIV and Bias at the Border
In 2019, a high-ranking US immigration official said that children of people living with HIV would be taken from their parents at the border because HIV is a "communicable disease." At least one father was separated from his three daughters for that reason. Again, people – including healthcare providers – organized against this policy. The official later changed his comments but insisted that HIV status could still play a role in case-by-case decisions on whether to separate children from their parents.
A variety of organizations help immigrants get legal advice, housing, food, basic necessities, and other services.
After a judge ordered separated families to be reunited, many children and parents had to provide samples of their DNA before they were brought together again. DNA is each person's unique biological code, which not only identifies the person, but also establishes relationship with close biological relatives. In 2020, under a new policy, ICE began to collect DNA from anyone it detains, including people legally applying for asylum. That biological information will be kept indefinitely in a database. In addition to identifying people, DNA can also tell whether someone is living with HIV. This could lead to further discrimination against people living with HIV who want to come to the US.
People suspected of being in the US without proper documentation are held in immigration detention centers. Many of these centers have little, if any, medical care, including HIV care. When people are arrested by ICE, any medication they have with them is taken away. Without access to healthcare providers, those in immigration detention cannot get their HIV medications. At least two women of transgender experience (trans women) living with HIV have died while held by ICE – one from complications from AIDS for lack of HIV drugs.
The US is again requiring people coming to the US-Mexico border to wait outside the US to apply for asylum ("Remain in Mexico" policy). The policy was originally announced in 2018 under then-President Donald Trump, rolled back by President Joe Biden's administration, but reinstated in December 2021. In theory, people "with known medical health issues" are exempt from that policy, but this may not be used in practice. Large tent camps have sprung up on the Mexican side of the border, with limited sanitation and even less medical care. Various organizations are trying to help, and some churches have set up shelters for waiting migrants. One such shelter, Albergue Las Memorias , is specifically for people living with HIV.
A variety of organizations help immigrants get legal advice, housing, food, basic necessities, and other services. Many are local or local chapters of national organizations. They are often affiliated with religious organizations, such as churches, but generally help people of any religion.
Less formally organized local groups may accompany immigrants to appointments, help with school enrollment or other bureaucratic tasks, provide referrals to clinics or HIV testing locations, or help with accessing other services. Some provide volunteer interpreters or help immigrants learn English.
Individuals not only volunteer with immigrant aid organizations and groups, but may host people in their homes, provide day-to-day support, including food and necessities, or donate money or goods to those providing direct support.
For an overview of the US Immigration system and advocacy to support immigrants, view our companion fact sheet, US Immigration and HIV: The Basics .

Become a Member
Join our community and become a member to find support and connect to other women living with HIV.
Join now >
You Might Also Like
- US Immigration and HIV: The Basics
- Women and HIV
- Housing Options for People Living with HIV in the US
- Public Benefits and HIV in the US
- Getting HIV Drugs in the US

Do you get our newsletter?
¿Recibe nuestro boletín?
Sign up for our monthly Newsletter and get the latest info in your inbox.
Suscríbase a nuestro boletín mensual y reciba la información más reciente en su bandeja de entrada.
You Can Help!
Together, we can change the course of the HIV epidemic…one woman at a time!
Please donate now!>
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 5 - Hepatitis E
- Section 5 - Influenza
Human Immunodeficiency Virus / HIV
Cdc yellow book 2024.
Author(s): Robyn Neblett Fanfair, Katarzyna (Kate) Buchacz, Philip Peters
Infectious Agent
Transmission, epidemiology, clinical presentation.
INFECTIOUS AGENT: Human immunodeficiency virus
TRAVELER CATEGORIES AT GREATEST RISK FOR EXPOSURE & INFECTION
PREVENTION METHODS
Avoid invasive procedures in locations where proper sterilization of instruments might not be used
Avoid nonsterile injection use
Practice safe sex
Take preexposure prophylaxis (for some travelers)
DIAGNOSTIC SUPPORT
HIV is an enveloped positive-strand RNA virus in the family Retroviridae .
HIV is transmitted through sexual contact, needle or syringe sharing, unsafe medical injection or blood transfusion, and organ or tissue transplantation. It can also be transmitted from mother to child during pregnancy, at birth, and postpartum through breastfeeding.
HIV infection occurs worldwide. In 2000, an estimated 37.7 million people were living with HIV infection globally . Sub-Saharan Africa is the most affected part of the world (25.4 million cases, or 67% of all people living with HIV infection); central Asia and eastern Europe have experienced the largest increases in new HIV infections (47% increase from 2010 to 2020). Although the reported adult HIV prevalence in many regions of the world is low, certain populations are disproportionately affected (e.g., sex workers, people who inject drugs, men who have sex with men, transgender people, and incarcerated people). People with HIV face an intersection of stigma, discrimination, violence, and criminalization that causes health inequities; international travelers should be aware of how their travel affects local communities, including people with HIV.
The risk for HIV infection is generally low for international travelers. Risk for HIV exposure and infection is determined less by a traveler’s geographic destination and more by the behaviors in which they engage while traveling (e.g., sex without a condom, nonsterile injection drug use). Travelers who might undergo scheduled or emergency medical procedures should be aware that HIV can be transmitted by unsafe nonsterile medical injection practices (e.g., reusing needles, syringes, or single-dose medication vials). Unsafe medical practices might be greater in low-income countries where the blood supply and organs and tissues used for transplantation might not be screened properly for HIV.
As many as 90% of infected people will recall experiencing symptoms during the acute phase of HIV infection. Acute HIV infection can present as an infectious mononucleosis-like or influenza-like syndrome, but the clinical features are highly variable. Symptoms typically begin a median of 10 days after infection and can include arthralgias and myalgias, fatigue, fever, headache, lymphadenopathy, maculopapular rash, malaise, oral ulcers, pharyngitis, and weight loss. Although none of these symptoms are specific for acute HIV infection, certain features (e.g., oral ulcers), suggest the diagnosis.
HIV can be diagnosed with laboratory-based or point-of-care assays that detect HIV antibodies, HIV p24 antigen, or HIV-1 RNA. In the United States, the recommended laboratory-based screening test for HIV is a combination antigen/antibody assay that detects antibodies against HIV, and the p24 antigen. The combination antigen/antibody assay becomes reactive approximately 2–3 weeks after HIV infection. Estimates suggest that 99% of people will develop a reactive combination antigen/antibody result within 6 weeks of infection, but in rare cases, it can take up to 6 months to develop a reactive test result.
HIV self-tests also are available for retail purchase in the United States, including an HIV antibody test performed on oral fluid instead of blood. Although oral swab HIV tests have a lower sensitivity for detecting recent HIV infection, these can be an important testing method for people and their partners who would not otherwise get an HIV test (see Sec. 11, Ch. 2, Rapid Diagnostic Tests for Infectious Diseases ). Acute HIV infection is characterized by markedly elevated HIV RNA levels; perform an HIV RNA viral load test if acute infection is suspected. Travelers with potential HIV exposures abroad, including those with symptoms consistent with acute HIV infection, should consider testing for HIV during travel or upon return to the United States. Travelers can find detailed information on HIV testing locations .
With timely diagnosis, prompt medical care, and daily antiretroviral therapy (ART), people with HIV can now live longer, healthier lives. Owing to the advances of ART, people with HIV who start treatment can have close to the same life expectancy as people of the same age without HIV. Effective treatment also substantially reduces the risk of transmitting HIV to others. People with HIV who achieve and maintain an undetectable viral load by taking ART daily as prescribed cannot sexually transmit the virus to others (undetectable = untransmittable [U = U]).
Detailed information on specific treatments is available from the Department of Health and Human Services HIVinfo website. Travelers can contact HIVinfo toll free at 800-448-0440 (English or Spanish) or 888-480-3739 (TTY).
Travelers can reduce their risk for HIV infection by avoiding sexual encounters with people whose HIV status is unknown, using condoms consistently and correctly with all partners who have HIV or whose HIV status is unknown, and using HIV prophylaxis when indicated. Travelers going abroad for medical procedures should try to ensure in advance that all blood or blood products at the facility have been screened for bloodborne pathogens (including HIV) and that all invasive medical equipment is sterilized between uses or is sterile and single use only (see Sec. 6, Ch. 2, Obtaining Health Care Abroad , and Sec. 6, Ch. 4, Medical Tourism ). Travelers who inject drugs should avoid sharing needles or other injection equipment and use only sterile, single-use syringes and needles that are safely disposed of after every injection.
Preexposure Prophylaxis
Preexposure prophylaxis (PrEP) is a highly effective method to prevent HIV acquisition and is used by people without HIV who are at risk of being exposed to HIV. Two medications have been approved by the US Food and Drug Administration for use as PrEP; each consists of 2 drugs combined in a single oral tablet taken daily. F/TDF (brand name Truvada) combines 200 mg emtricitabine with 300 mg tenofovir disoproxil fumarate. F/TAF (brand name Descovy) combines 200 mg emtricitabine with 25 mg tenofovir alafenamide.
People already on PrEP should continue its use during international travel. Travel medicine providers can consider initiating PrEP for people who have a greater risk for HIV acquisition [PDF] during international travel. A comprehensive prevention plan includes not only prescribing (or considering prescribing) PrEP, but also reinforcing careful adherence to the PrEP regimen, educating travelers on the importance of consistent condom use to protect against HIV as well other sexually transmitted infections, and discussing other HIV prevention methods.
Travelers taking PrEP should carry proper documentation and be aware that some countries (see below for further information) deny entry to people with evidence of HIV infection, which PrEP medications might mistakenly indicate to customs officials. Free, expert PrEP advice is available to health care professionals through the National Clinician Consultation Center’s PrEPline (855-448-7737).
Postexposure Prophylaxis
Postexposure prophylaxis (PEP) with antiretroviral medications is another method to prevent HIV infection. PEP is recommended as a prevention option after a single high-risk exposure to HIV during sex, through sharing needles or syringes, through a needlestick, or from a sexual assault. PEP must be started within 72 hours of a possible exposure. Travelers who will be working in medical settings (e.g., nurse volunteers drawing blood, medical missionaries performing surgeries) could have contact with HIV-infected or potentially infected biological materials.
Under certain conditions, a clinician can prescribe PEP medications for travelers to use in emergency situations. Free, expert PEP advice is available to health care professionals through the National Clinician Consultation Center’s PEPline (888-448-4911). See Sec. 9, Ch. 4, Health Care Workers, Including Public Health Researchers & Medical Laboratorians , for detailed advice regarding management of postexposure prophylaxis in occupational settings.
HIV Testing Requirements for US Travelers Entering Foreign Countries
Advise international travelers that some countries screen incoming travelers for HIV (usually those with an extended stay) and might deny entry to people with evidence of HIV infection. People intending to visit a country for an extended stay should review that country’s policies and requirements. This information is usually available from the consular officials of the individual nations. The US Department of State has compiled a list of entry, exit, and visa requirements by country .
CDC website: HIV
The following authors contributed to the previous version of this chapter: Philip J. Peters, John T. Brooks
Bibliography
Brett-Major DM, Scott PT, Crowell TA, Polyak CS, Modjarrad K, Robb ML, et al. Are you PEPped and PrEPped for travel? Risk mitigation of HIV infection for travelers. Trop Dis Travel Med Vaccines. 2016;2:25.
Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV in the United States–2017 update: a clinical practice guideline. Atlanta: The Centers; 2018. Available from: www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf [PDF].
Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV in the United States–2017 update: clinical providers’ supplement. Atlanta: The Centers; 2018. Available from: www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-provider-supplement-2017.pdf [PDF]
Centers for Disease Control and Prevention. HIV and COVID-19 Basics. Available from: www.cdc.gov/hiv/basics/covid-19.html .
Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS data 2020. Geneva: UNAIDS; 2020. Available from: www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf [PDF].
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in adults and adolescents with HIV. Washington, DC: Department of Health and Human Services; 2021. Available from https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/AdultandAdolescentGL.pdf [PDF].
Patel P, Borkowf CB, Brooks JT, Lasry A, Lansky A, Mermin J. Estimating per-act HIV transmission risk: a systematic review. AIDS. 2014;28(10):1509–19.
World Health Organization. Coronavirus disease (COVID-19): COVID-19 vaccines and people living with HIV. Available from: www.who.int/news-room/q-a-detail/coronavirus-disease-(covid-19)-covid-19-vaccines-and-people-living-with-hiv .
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Cookies in use
days left to the 2024 election! Your ballot is your power, and when we show up, equality wins. Click here to visit our 2024 Voting Center!
After 22 Years, HIV Travel and Immigration Ban Lifted
by HRC Staff • January 4, 2010
"The United States of America has moved one step closer to helping combat the stigma and ignorance that still too often guides public policy debates around HIV/AIDS," said HRC President Joe Solmonese.
Washington - The Human Rights Campaign, the nation's largest lesbian, gay, bisexual and transgender (LGBT) civil rights organization, hailed the announcement that a ban on HIV positive visitors and immigrants entering the country, first established in 1987, has been lifted. A regulation promulgated by the Obama administration last summer and finalized in November goes into effect today, removing HIV from the list of communicable diseases that bar foreign nationals from entering the United States.
"The United States of America has moved one step closer to helping combat the stigma and ignorance that still too often guides public policy debates around HIV/AIDS. Today, a sad chapter in our nation's response to people with HIV and AIDS has finally come to a close and we are a better nation for it," said HRC President Joe Solmonese."This policy, in place for more than two decades, was unnecessary, ineffective and lacked any public health justification."
In July 2008, President Bush signed into law, as part of the reauthorization of the President's Emergency Plan for AIDS Relief (PEPFAR), a provision that removed the ban from statute and returned regulatory authority to the Secretary of Health and Human Services to determine whether HIV should remain on a list of communicable diseases that bar foreign nationals from entering the United States.
HRC has been a lead organization lobbying on Capitol Hill for the statutory repeal and working to ensure that Department of Health and Human Services' regulations were changed. The Human Rights Campaign worked closely with the offices of Senator John Kerry (D-MA) and former Senator Gordon Smith (R-OR), as well as Rep. Barbara Lee (D-CA), the sponsors of the effort in Congress last year to repeal the ban. After the passage of the PEPFAR bill, HRC lobbied both the Bush and Obama administrations to remove the remaining regulatory ban. In July 2009, when the proposed regulation lifting the ban was open for public comment, more than 19,000 HRC members and supporters submitted statements in favor of ending the discriminatory policy.
The travel and immigration ban prohibited HIV-positive foreign nationals from entering the U.S. unless they obtained a special waiver, which was difficult to secure and then only allowed for short-term travel. The policy also prevented the vast majority of foreign nationals with HIV from obtaining legal permanent residency in the United States. The ban originated in 1987, and was explicitly codified by Congress in 1993, despite efforts in the public health community to remove the ban when Congress reformed U.S. immigration law in the early 1990s. While immigration law currently excludes foreigners with any "communicable disease of public health significance" from entering the U.S., only HIV had been explicitly named in the statute.
The Human Rights Campaign is America's largest civil rights organization working to achieve lesbian, gay, bisexual and transgender equality. By inspiring and engaging all Americans, HRC strives to end discrimination against LGBT citizens and realize a nation that achieves fundamental fairness and equality for all.
To make a general inquiry, please visit our contact page. Members of the media can reach our press office at: (202) 572-8968 or email [email protected].
Love conquers hate.
Let's win this..
100% of every HRC merchandise purchase fuels the fight for equality.
Choose a Location
- Connecticut
- District of Columbia
- Massachusetts
- Mississippi
- New Hampshire
- North Carolina
- North Dakota
- Pennsylvania
- Puerto Rico
- Rhode Island
- South Carolina
- South Dakota
- West Virginia
Leaving Site
You are leaving hrc.org.
By clicking "GO" below, you will be directed to a website operated by the Human Rights Campaign Foundation, an independent 501(c)(3) entity.

HIV-related travel restrictions
- Press release
- Personal stories
- Infographic
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Which Countries Restrict Travel to People With HIV?
It was only in 2010 that the United States finally lifted its 22-year ban on travelers with HIV , a law that prohibited all infected persons from obtaining tourist visas or permanent residence status in the U.S.. The order, initiated by George H.W. Bush in 2008, was made official by Barack Obama on January 4, 2010.
While efforts are being made to end similar laws throughout the world, the Global Database on HIV-Specific Travel & Residence Restrictions (a joint European initiative published by the International AIDS Society) reports that as of 2023, 56 out of 200 countries are known to have entry regulations for people living with HIV, and seven of these countries will categorically refuse entry without exception. In some of these countries, entry may be allowed, but there are restrictions depending on the length of stay. For example, 54 countries have restrictions on stays over 90 days (student and work visas); whereas less than 10 countries have laws that can affect travelers visiting for less than 90 days (tourists). Furthermore, 18 of these countries will deport visitors discovered to have HIV.
HIV Travel Restrictions in Practice
It is important to note, however, that there is often a lack of clarity about these laws, with some either not addressing HIV directly (describing only "infectious disease" concerns) or not enforcing the laws all that stringently, if at all. As such, the assessments provided below are couched in terms that best reflect whether an action "will," "can" or "may" take place.
Similarly, there is a lack of clarity about the import of antiretroviral drugs —whether the drugs are allowed for personal use; how much can be brought in if they are permitted; or if possession of such constitutes the right to deny entry.
For these reasons, it is advised that you always speak with the consulate or embassy of any of the listed destinations if you plan to visit.
Countries With Restrictions for People Living with HIV
Algeria (>90 days)
Aruba (>90 days)
Australia (>90 days)
Azerbaidjan (>90 days)
Bahrain (>90 days)
Belize (>90 days)
Bhutan (>2 weeks)
Bosnia Herzegovina (>90 days)
Brunei (no entry, will deport)
Cayman Islands (>90 days)
China (>90 days, will deport)
Cuba (>90 days)
Cyprus (>90 days)
Dominican Republic (>90 days)
Egypt (>90 days, will deport)
Equatorial Guinea (no entry, will deport)
Honduras (>90 days)
Iran (>90 days)
Iraq (>10 days, possible deportation)
Israel (>90 days)
Jordan (no entry, will deport)
Kazakhstan (>90 days)
Kuwait (>90 days, will deport)
Kyrgyzstan (>60 days)
Lebanon (>90 days, will deport)
Malaysia (>90 days, will deport)
Marshall Islands (>30 days)
Mauritius (>90 days)
Montserrat (>90 days)
Nicaragua (>90 days)
North Korea (will deport)
Oman (>90 days, will deport)
Papua New Guinea (>6 months)
Paraguay (>90 days)
Qatar (>1 month, will deport)
Russia (>90 days, will deport)
Samoa (>90 days)
Saudi Arabia (>90 days, will deport)
Seychelles (>90 days)
Singapore (>90 days)
Slovakia (>90 days)
Solomon Islands (no entry, will deport)
St. Kitts and Nevis (>90 days)
St. Vincent and Grenadines (>90 days)
Sudan (>90 days)
Suriname (entry restrictions)
Syria (>90 days, will deport)
Tonga (>90 days)
Tunisia (>30 days)
Turks and Caicos Islands (>90 days)
United Arab Emirates (UAE) (no entry, will deport)
Uzbekistan (>90 days)
Virgin Islands (>90 days)
Yemen (no entry, will deport)
Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services (HHS). Medical examination of aliens—Removal of human immunodeficiency virus (HIV) infection from definition of communicable disease of public health significance. Final rule . Fed Regist. 2009;74:56547–56562.
The Global Database on HIV-Specific Travel & Residence Restrictions. Regulations on entry, stay and residence for PLHIV .
By James Myhre & Dennis Sifris, MD Dr. Sifris is an HIV specialist and Medical Director of LifeSense Disease Management. Myhre is a journalist and HIV educator.

I am HIV positive, can I travel to the USA?
30 April 2012. Related: All topics , Travel .
Hi – I have two questions:
1. Can I travel to the USA if I am positive? If so, must I tell the airport authorities what my drugs are if they stop me? If so, will this be noted on my record anywhere? Or passport?
2. I normally take my meds at 8am (UK time). How do I change the time and to what now that I am going to the USA? I will be 5 hours behind which means I would need to take them at 3am which isn’t practical.
Answer: Rebecca McDowall
Thank-you for your question.
There are no travel restrictions for HIV positive people traveling to the USA. All American travel restrictions relating to HIV status were lifted in January 2010.
Customs regulations require people entering with prescription medication like antiretroviral drugs to carry a doctor’s certificate in English, stating that the drugs are required to treat a personal condition. This requirement applies to all prescription drugs, not just HIV treatment.
Medication should always be carried in hand luggage, as checked luggage may be delayed or get lost. If you are carrying-on liquid medication exceeding 3 ounces / 100 ml, you must declare it at the checkpoint for inspection.
As for what time to take your medication, this really depends on which ARVs you are taking. For answers to similar questions please follow the links below:
I’m moving from Asia to Europe- when do I take my meds?
Can I occasionally stretch my atazanavir dose to 32 hours?
How do I time my meds when travelling?
174 comments
Hi Josephine, yes you can travel to Canada. Being HIV positive will not prevent you travelling.
You can see here for more information: https://www.hivtravel.org/Default.aspx?PageId=143&CountryId=39
Can I travel to Canada and iam HIV positive
Hi Theju, this is fine in many countries, including in the UK. Sometimes it is good to also have a doctors letter that say they need these meds, just in case it is needed. Please also check this website for restrictions in a few countries: http://www.hivtravel.org
Your email address will not be published. Required fields are marked *

An official website of the United States government
Here’s how you know

Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

This page was published more than five years ago. Information on the page may be out of date.
- For International Visitors
- Electronic System For Travel Authorization
Final Rule Removing HIV Infection from U.S. Immigration Screening
Effective January 4, 2010, a diagnosis of HIV infection will not render a person traveling into the United States as inadmissible under Section 212(a)(1)(A)(i) of the Immigration and Nationality Act (INA). Thus, HIV-positive travelers seeking entry to the United States no longer need a waiver of inadmissibility to travel to the United States.
This includes travelers who successfully obtained a waiver of inadmissibility for HIV infection in the past and those who were denied admission into the United States based on HIV infection and the lack of a waiver of inadmissibility thereof.
Travelers from Visa Waiver Program (VWP) countries who were previously denied an approved Electronic System for Travel Authorization (ESTA) based solely on HIV infection would not be barred from re-applying for travel authorization and their HIV infection would no longer bar them from receiving an ESTA authorization.
Additionally, effective January 4, 2010, CBP officers shall not consider a lack of HIV test results when making a determination of admissibility on an arriving immigrant or refugee.
HIV-positive travelers who have any other grounds of inadmissibility under Section 212(a) of the INA must continue to obtain a waiver of inadmissibility.
CBP strives to treat all travelers with respect and in a professional manner, while maintaining the focus of our mission to protect all citizens and visitors in the United States.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- How It Spreads
- Living with HIV
- HIV Awareness Days
- HIV in the United States
- Resource Library
- Occupational Exposure
- Connect With Us
Related Topics:
- View All Home
- HIV Nexus: CDC Resources for Clinicians
- HIV Public Health Partners
- Ending the HIV Epidemic in the U.S. (EHE)
- Let's Stop HIV Together
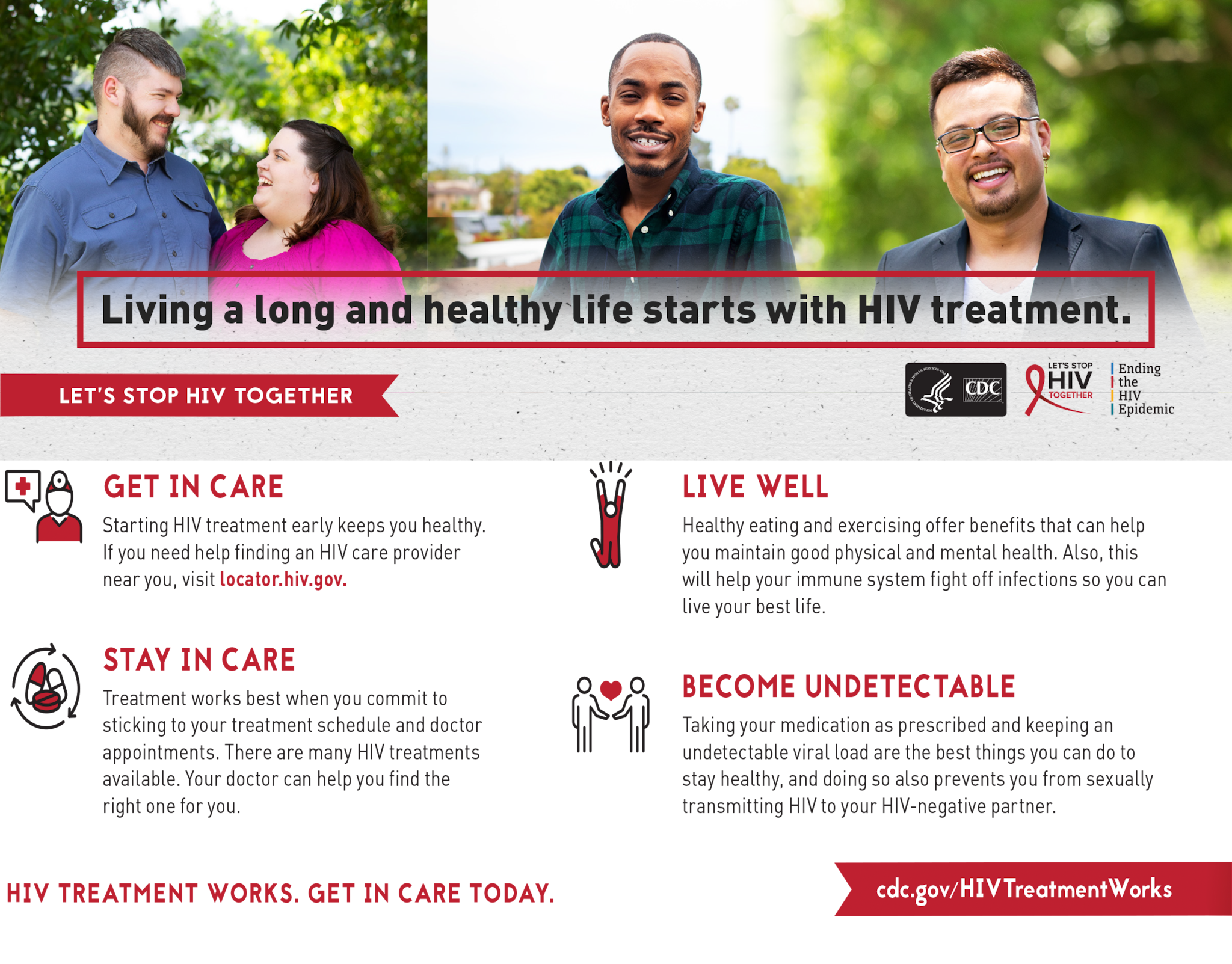
- HIV is manageable like many other chronic diseases.
- Once you have HIV, you have it for life. Unlike some other viruses, you can't get rid of HIV completely.
- People with HIV who get treatment can live long, healthy lives, and protect others.

Newly diagnosed with HIV
Receiving an HIV diagnosis can be life changing. You may feel many emotions—sadness, hopelessness, or anger. Health care providers and social service providers can help you find HIV care and navigate the early stages of your diagnosis.
Find HIV care
A health care team that is knowledgeable about HIV care will help you manage your care and treatment. Your primary HIV care provider should lead your health care team.
You can also use the locator below to find a local health center or a Ryan White HIV/AIDS provider who can help you access medical care, medications , and essential support services.
Start HIV treatment as soon as possible
HIV treatment (antiretroviral therapy or ART) involves taking medicine to reduce the amount of HIV in your body. When taken as prescribed, HIV medicine can make the amount of virus in your body ( viral load ) so low that a test can't detect it ( undetectable viral load ). Getting and keeping an undetectable viral load is the best thing people with HIV can do to stay healthy.
Protect others
There are many actions you and you partners can take to prevent HIV transmission.
Having an undetectable viral load prevents HIV transmission during sex. But there are situations when either partner may want to use additional prevention options.
- Using condoms can help prevent other STIs, like gonorrhea and chlamydia.
- Using condoms or having your partner take PrEP (pre-exposure prophylaxis) can provide added peace of mind.
- Are unsure, for any reason, that you have an undetectable viral load;
- Have a high viral load (200 copies of HIV per milliliter of blood or greater);
- Have trouble taking HIV medicine regularly;
- Missed some doses since your last viral load test; or
- Have stopped taking HIV medicine or may do so in the future.
A small number of people can’t get an undetectable viral load even though they take HIV medicine as prescribed. You can still protect your partners by using other HIV prevention options.
Telling others
In some states, there are laws that require you to share your HIV status with your sex or injection partners. Sharing your status with anyone else is your choice.
Sex or injection partners
Telling your partners that you have HIV before you have sex or inject drugs helps your partners make decisions to protect their health. You should also tell your partner(s) if you've been diagnosed with another STI so they can get tested.
There are two ways to let your partner(s) know:
- You tell your partner(s). These conversations can be hard. A partner may have exposed you to HIV, or you may have exposed them without knowing. For tips on how to tell your partner, check out the conversation starters from Let's Stop HIV Together .
- The health department tells your partner(s). This is sometimes called "Partner Services." In addition to letting them know they may have been exposed to HIV, they will also provide your partners with testing, counseling, and referrals for other services. Your health care provider, social worker, case manager, patient navigator, or HIV testing center can help you find a Partner Services program.

Health care providers
Health care providers and other HIV service providers need to know about your HIV diagnosis, so they make sure you get the services you need.
Family and friends
Sharing your HIV status with certain family members and friends has many benefits.
- Your family and friends can help you deal with an HIV diagnosis.
- They can support you with treatment challenges.
- They can help you disclose your status to others.
- They can speak for you in case of an emergency.
- They can help you navigate the medical system.
You do not have to tell your employer. But you may want to in case you need to take extended leave or change your schedule.
By law, your disclosure is confidential. Learn about disclosure, confidentiality, and the law . Your state health department can also share your state's laws and how they apply to disclosure.
Healthy living
In addition to taking your HIV treatment and seeing your health care provider, there are ways to keep yourself healthy and your immune system strong.
Eat healthy and exercise
Following a healthy diet provides the energy and nutrients you need to fight HIV and other infections. Talk to your health care provider about your diet and ask about steps you can take to maintain good nutrition. Exercise helps you maintain good physical and mental health and helps your immune system fight infections. Find a fitness routine that you enjoy.
Stay up to date with health screenings and vaccinations
People with HIV have an increased chance of developing severe symptoms from common infections. Staying up to date on routine screenings and vaccines can help you prevent infection or severe disease.
Prevent illnesses
Some illnesses (sometimes called opportunistic infections) occur more often and are more severe in people with HIV. Common severe illnesses include herpes simplex virus, tuberculosis, or pneumonia.
Today, severe illnesses are less common because of effective HIV treatment. Taking HIV medicine as prescribed is the best way to keep your immune system strong and healthy. Talk to your health care provider about things that could expose you to illnesses at work, at home, and on vacation. If you get an illness, talk to your health care provider about how to treat it.
Quit smoking
People with HIV who smoke are more likely than those who don't smoke to develop cancers, pneumonia, chronic obstructive pulmonary disease, and heart disease. Smoking is also linked to poorer response to HIV treatment.
For support in quitting, call 1-800-QUIT-NOW (1-800-784-8669).
Taking care of your mental health
Having HIV can be a source of major stress. HIV may challenge your sense of well-being or complicate existing mental health conditions. Good mental health will help you live your life to the fullest and is essential to successfully treating HIV.
Ask your health care provider, social worker, or case manager about local support groups. They may also refer you to a mental health provider who can give you the care you need.
Traveling with HIV
Traveling outside the United States may require special precautions for people with HIV. For example, travel to some countries can increase the chances of getting an severe illness.
Before you travel
- Discuss medicine and vaccines with your health care provider at least 4 to 6 weeks before you travel.
- Check your medical insurance for travel coverage. Consider purchasing additional travel insurance if your insurance doesn't cover emergency care or transportation in other countries.
- Learn about the health risks in the places you plan to visit. Find out if the countries you plan to visit have special health rules for visitors with HIV.
During travel
- Learn how to incorporate safer eating and drinking habits to reduce your chances of getting sick when you travel.
- Avoid direct contact with animals and animal waste (stool) . Animal stool in soil, water, or on sidewalks can be harmful to people with HIV.
- Avoid hospitals and clinics where coughing tuberculosis (TB) patients are treated. See your health care provider when you return to discuss whether you should be tested for TB.
Resources and support
Find hiv care and treatment.
- Find HIV care services near you . Find local HIV medical care, housing assistance, and substance abuse and mental health services.
- Find your state HIV/AIDS toll-free hotline . Connect with agencies that can help determine what services you are eligible for and help you get them.
- Search for HIV care specialists . Find HIV providers who are members of the American Academy of HIV Medicine.
Get help paying for HIV care
- Find out if you're eligible for the Ryan White HIV/AIDS Program . See if you qualify for assistance with medical care and other essential support services.
- See if you qualify for disability benefits . If you have HIV and cannot work, you may qualify for benefits from the Social Security Administration.
- Estimate the cost of health coverage . Use online cost calculators to help you understand options for lowering the cost of health insurance.
- Find out how to get Medicare drug coverage . If you have Medicare, learn about what the drug plans cover and the costs you'll pay.
- Get affordable health insurance . See if you can enroll in or change plans and get answers to common questions.
- Learn about the Affordable Care Act (ACA) . The ACA created several changes that expand access to coverage for people with HIV.
- Learn about Patient Assistance and Expanded Access Programs . Find prescription drug assistance information and learn about current expanded access trials.
Find housing and job resources
- L earn about the Housing Opportunities for Persons With AIDS (HOPWA) Program . HOPWA is the only Federal program dedicated to addressing the housing needs of people with HIV.
- Find affordable housing opportunities . If you are homeless, at risk of becoming homeless, or know someone who is, you might be eligible for housing assistance.
- Find questions and answers about housing assistance . Find out what housing programs are available for people with HIV and learn about eligibility requirements.
- Get advice on getting a new job or returning to work . Find out how to return to work and learn about your right to request reasonable accommodations.
- Find resources on employment options for people with HIV . View toolkits, read success stories, and find resource guides for entering or returning the workforce.
Get help with legal issues
- Find states that have HIV-specific criminal laws . Access resources about disclosure, confidentiality, and the law from the Center for HIV Law and Policy.
- Get information about HIV discrimination . Learn about how the Americans with Disabilities Act (ADA) protects people who are discriminated against because they have HIV or have a relationship with someone with HIV.
- File an HIV discrimination complaint . File an ADA complaint related to HIV discrimination in employment or housing.
Find mental health treatment
- Find mental health treatment programs . View a list of organizations and contact numbers that can help you find mental health treatment and support in your local area.
- Learn about depression . Get information about depression's causes, symptoms, and treatments.
Learn about HIV stigma and discrimination
View testimonials about dealing with stigma . CDC's Let's Stop HIV Togethe r campaign has resources to help start conversations about stigma with your friends, family, and community.
Find traveling resources
- Learn about travel health guidelines for immunocompromised travelers . CDC's Yellow Book provides pretravel vaccine recommendations and destination-specific health advice.
- Get travel advice and resources . CDC's Travelers' Health page helps you locate travel clinics near you, get travel notices for your destination, and learn about vaccinations and precautions.
Get information on older adults with HIV
- Access the latest data on HIV and older Americans from the CDC.
- Get more information on HIV and older people from the National Institute on Aging.
Living with HIV 101
HIV Treatment is HIV Prevention
Treatment Palm Card

Undetectable Palm Card
Learn about HIV and how the virus is transmitted, how to protect yourself and others, and how to live well with HIV. Also learn how HIV impact the American people.
- Persecution
- Physical Presence
- One-Year Filing Deadline
- Criminal Bars to Asylum
- Passing a Credible/Reasonable Fear Interview
- Withholding of Removal
- Convention Against Torture Relief
- Application Process
- Work and Travel While Pending
- Case Outcome
- Important Changes for Asylum Seekers under the Trump Administration
- Asylum Manual
- Self-Help Asylum Guides
People Living with HIV
- Foreign-born Children of Same-Sex Couples
- Bi-national Couples
- Dual Foreign-national Couples
- Diversity Visa Program
- Provisional Unlawful Presence Waiver
- Deferred Action for Childhood Arrivals (DACA)
- Violence Against Women Act
- Special Immigrant Juvenile Status
- Know Your Rights!
- Country Conditions Materials
- ALERT: USCIS FEE INCREASES GO INTO EFFECT (October 2, 2020)
- Report: The Mistreatment of LGBTQ People in U.S. Federal Immigration Jails
The information contained herein is for reference only and may not be up to date. It does not constitute legal advice. You should always consult an attorney regarding your matter.
Last updated: June 3, 2020
One of Immigration Equality’s core principles is to ensure that U.S. immigration law does not discriminate or stigmatize people living with HIV. At the same time, we are often successful in securing asylum for people living with HIV who fear persecution on that basis. Anyone thinking about applying for asylum based on HIV status should review our asylum materials carefully and also consult with an experienced immigration attorney.
Asylum Based on HIV-Status
In some countries it is dangerous to be a person living with HIV. While the Board of Immigration Appeals has confirmed that persecution because of sexual orientation is a reason someone might be granted asylum, there is no similar decision by an appeals court overtly acknowledging HIV-related persecution as a basis for asylum. Nevertheless, there have been many cases where individuals have been granted asylum solely because of their HIV status. In general, to win asylum, an individual must prove “persecution” not “hardship,” and so in most cases it would not be sufficient to show that HIV medication would not be available because their country or origin cannot afford medicine. To learn more please read this article on HIV-based asylum applications. Also, in 1996 INS issued a memo describing circumstances under which people living with HIV might qualify for asylum. Finally, the asylum officer’s basic training manual notes that an asylum claim “may” be a basis for protection. For more information on the asylum process, please see our section on asylum .
Persons living with HIV who fear mistreatment because of HIV-related stigma in their country of origin should consult with an experienced immigration attorney.
Family-based Immigration
On January 4, 2010, the Department of Health and Human Services (HHS) final regulations went into effect, removing HIV from its list of “communicable diseases of public health significance” and removing the HIV test from the routine medical exam for lawful permanent resident applicants. Additionally, while applying for lawful permanent residence, use of some benefits such as the AIDS Drug Assistance Program did not historically count against an applicant when the government makes a determination on whether a person will likely be a public charge . However, regulations issued in 2020 may have changed that. For more information, see this update .
People Living with HIV in Immigration Detention
Conditions for people living with HIV in ICE or CBP detention are deplorable. Detention facilities often deny or delay HIV medications, give incorrect dosage of HIV medications, or do not allow someone to refill their HIV medications. In fact, in 2019, ICE separated a man living with HIV from his children because the officers thought that he might accidentally transmit the illness to them. For information on conditions in detention and recourses, please see our resources on detention .
Other HIV-based Immigration
Prior to changes in the immigration law in 1996, it was possible for undocumented foreign nationals who had been in the U.S. for long periods of time and could prove extreme hardship if they would be deported, to obtain lawful permanent residence through “suspension of deportation.” That immigration benefit no longer exists. It was replaced by “cancellation of removal” which allows certain undocumented foreign nationals to obtain lawful permanent residence, but only if they can show extreme and exceptionally unusual hardship to their United States citizen or lawful permanent resident immediate relatives. Hardship to one’s self is no longer recognized as a ground to gain lawful permanent residence.
In very limited circumstances, the Department of Homeland Security (DHS) can grant “deferred action” status meaning that it gives permission for a foreign national to remain in the U.S. temporarily because of an extremely compelling humanitarian circumstance such as a late stage terminal illness. (Note that this form of “deferred action” is distinct from Deferred Action for Childhood Arrivals, (DACA,) which is available to certain individuals who arrived in the United States as children and who meet other eligibility requirements.) An individual living with HIV who fears that they would not live very long if they are returned to their country of origin due to lack of availability of treatment, may consider applying for deferred action. It should be noted that deferred action is a discretionary relief and is granted on a case-by-case basis. Most applications are denied. Anyone considering a deferred action application should consult with a qualified immigration attorney before doing so.
Applicants lacking valid immigration status who apply for deferred action run a real risk that their requests will be denied, and that Immigration and Customs Enforcement will take steps to remove them from the United States.
Historical Summary – HIV Ban Was Lifted
From 1993 until January 4, 2010, HIV was considered a ground of inadmissibility, meaning that HIV-positive foreign nationals could be denied short-term visas or applications for lawful permanent residence simply because of their HIV status. Fortunately, with the help of Immigration Equality and our coalition partners, that discriminatory law came to an end in the beginning of 2010.
On January 4, 2010, the HIV ban on travel and immigration, which had been in place for two decades finally came to an end. With the end of the HIV ban, being HIV positive is no longer an automatic ground of “inadmissibility.” For foreign nationals seeking to enter as tourists or short-term visitors, being positive should not be an issue at all. For lawful permanent resident applicants, being HIV-positive could still affect USCIS’s determination about whether someone is “likely to become a public charge.” While doctors will no longer perform an HIV antibody test as part of the medical examination, the doctor could ask questions about overall health which could lead the doctor to conclude that someone is HIV positive. While it is not necessary to volunteer information about HIV status, always be honest with the doctor performing the medical exam. In addition, immigration and consular officials are permitted to take health into account when determining whether an applicant is likely to need government assistance, which can be a ground for denying a green card application.
Historical Information and Links to Important Documents
After a 60 day waiting period, the final regulations which were published by the Department of Health and Human Services on November 2, 2009, became law. The regulations removed HIV from the list of “communicable diseases of public health significance,” meaning that anyone seeking to enter the U.S. as a visitor can do so without having to disclose their HIV status. The regulations also remove the HIV testing requirement for lawful permanent resident applicants.
As the lengthy bureaucratic process of publishing the regulations and issuing guidance on their implementation unfolded, there were several significant memoranda be issued by various U.S. government agencies about the end of the ban. The United States Citizenship and Immigration Services issued two memos about implementation of the end of the ban. On September 15, 2009 USCIS issued a memo which provided guidance on adjudicating cases before the January 4, 2010 change in the law. Specifically, the memo instructed officers not to deny cases based solely on a person’s HIV-positive status, but rather to hold them in abeyance until the change in the law.
On November 24, 2009, USCIS issued further guidance to its officers on adjudicating cases after January 4, 2010. Namely, the memo reiterates that HIV will no longer be a ground of inadmissibility, that waivers for individuals with HIV will no longer be required, that HIV anti-body testing will no longer be a part of the medical exam for lawful permanent resident applicants. It also provided that upon a motion with the proper fee, applications that were denied solely because the applicant was HIV positive after July 2, 2009 (the date that the final regulations were published) may be reopened.
At long last, on December 17, 2009, the Department of State issued a Q and A explaining the end of the HIV ban. This is very important because individuals seeking visas abroad (either short-term or for permanent residence) must do so with U.S. consulates which are part of DoS, not USCIS. The guidance made it clear that after January 4, 2010, HIV was no longer a reason to deny visas. However, if any problems with a consulate arise, please contact Immigration Equality.
Also, the Centers for Disease Control issued a letter to all doctors who conduct immigration medical exams. USCIS has updated the I-693 form to eliminate the box for HIV testing. Some doctors, however, may test for HIV with an applicant’s consent. If a physician does test for HIV, or if an applicant discloses their HIV status, the physician may record the HIV status on the I-693. It is important to note, however, that an indication or diagnoses of HIV, alone, will not affect visa or immigration applications.
The end of the HIV ban was the culmination of remarkably hard work by a broad coalition of immigration, HIV, LGBTQ, and human rights organizations. Together, we mobilized over 23,000 comments in favor of lifting the ban with fewer than 550 comments against lifting the ban. Significantly, over 400 organizations submitted or signed onto comments calling for an end to the ban and there were no organizational comments that asked HHS to keep the ban in place. Immigration Equality was among the organizations that submitted comments in full support of the proposed regulations.
None of this would have been possible without the leadership of Senators John Kerry and Gordon Smith and Congresswoman Barbara Lee, who led the fight in Congress in 2008 to remove the statutory HIV ban.
If you’ve looked through our legal resources and still have questions, please reach out via one of our contact forms at the bottom of this page .
This handbook is intended for use by pro bono attorneys and immigration attorneys working on LGBTQ/HIV asylum cases.
Self-help asylum guides for LGBTQ and HIV-positive people without attorneys.
- Doctors, Clinics & Locations, Conditions & Treatments
- Patients & Visitors
- Medical Records
- Support Groups
- Help Paying Your Bill
- COVID-19 Resource Center
- Locations and Parking
- Visitor Policy
- Hospital Check-in
- Video Visits
- International Patients
View the changes to our visitor policy
View information for Guest Services
New to MyHealth?
Manage Your Care From Anywhere.
Access your health information from any device with MyHealth. You can message your clinic, view lab results, schedule an appointment, and pay your bill.
ALREADY HAVE AN ACCESS CODE?
Don't have an access code, need more details.
Learn More about MyHealth Learn More about Video Visits
MyHealth for Mobile
Get the iPhone MyHealth app Get the Android MyHealth app
WELCOME BACK
Traveling with hiv.

For people with HIV, travel can pose specific risks. According to the CDC, travel, especially to developing countries, can increase the risk of contracting opportunistic infections. These infections are referred to as opportunistic because a person's weakened immune system gives the infection the opportunity to develop. The risk varies according to the CD4 cell count. People at highest risk are those with a CD4 cell count of less than 200 per cubic millimeter or a history of an AIDS-related illness.
Special precautions that should be taken if you are traveling with HIV include the following:
- Consult your doctor or a travel medicine expert as early as possible about the health risks that exist in the areas you plan to visit. Your doctor can offer suggestions about staying healthy in places where certain illnesses may pose special threats. Ask for names of doctors who treat HIV in the regions you plan to visit.
- During travel to developing countries, people infected with HIV are at a much higher risk for food and waterborne disease than they are in the United States. Take extra precautions to avoid any uncooked foods and make sure all water is either boiled or bottled.
- Traveler's diarrhea is a common problem. Carry a three- to seven-day supply of medicine to treat it. Consult your doctor for more information on appropriate medication for you.
- Waterborne infections may also result from swallowing or even being exposed to some bodies of water during recreational activities. Reduce your risk of these infections by being careful to not swallow water while swimming, and to avoid swimming or wading in water that may be contaminated.
- Take precautions against insect-borne diseases in areas where this is a problem. Use insect repellents with DEET and mosquito-netting treated with permethrin while sleeping in areas where malaria, dengue fever, or other insect-borne diseases are prevalent. People with HIV infections are urged to avoid areas where yellow fever is found.
- Tuberculosis is very common worldwide and can be very serious in people with HIV. Avoid hospitals and clinics where tuberculosis patients are treated and be sure to be tested when you return to the United States.
- Take all medications as prescribed by your doctor. Make sure you bring enough to last throughout your trip and written prescriptions for refills in case of emergency.
- If you are on a special diet, adhere to your meal plan as much as possible while traveling.
- Take all of the same precautions that you take at home to prevent transmitting HIV to others.
Immunization information for persons with HIV
Ask your doctor about special vaccinations that may be necessary before you travel. Make sure all of your routine immunizations are up-to-date. This is especially important for children with HIV who are traveling.
Consult your doctor or the CDC for more information regarding specific immunizations you may need before you travel.
Condition Spotlight

Clinical Trials
Clinical trials are research studies that evaluate a new medical approach, device, drug, or other treatment. As a Stanford Health Care patient, you may have access to the latest, advanced clinical trials.
Open trials refer to studies currently accepting participants. Closed trials are not currently enrolling, but may open in the future.
Clinics for Traveling with HIV
- Infectious Diseases Clinic 650-736-5200
- Positive Care Clinic 650-723-9001
U.S. Ban on HIV-Positive Visitors, Immigrants Expires
Health experts say the 22-year ban reflected ignorance about disease.
WASHINGTON, Jan. 5, 2010— -- In a move public health and human rights advocates have hailed as a "victory," the so-called HIV travel ban, which barred entry to the U.S. by people living with HIV or AIDS, has been officially revoked, bringing to a close years of work to end the measure.
"I think there's reason to be joyful that the ban has been lifted because a ban like this sends the message that somehow we're going to protect ourselves from HIV by not letting people with HIV come into the country," Dr. Tom Coates, a UCLA global health expert, told ABC News. "And the truth of the matter is that's not how we protect ourselves from HIV."
For more than 20 years, people living with HIV or AIDS needed look no further than the United States' front door for a reminder of the stigma associated with their disease. A U.S. immigration measure first imposed in 1987 after politicians reacted to the outbreak of AIDS prohibited all infected persons from obtaining U.S. tourist visas or permanent residence status unless they obtained a special waiver.
Coates said the ban created a "false security" and fueled misunderstanding that public health and prevention programs are the best way to curb spread of the disease.
President George W. Bush began the process to repeal the ban in 2008, and in October, President Obama took the final steps to complete the move. The repeal took effect on Monday.
"If we want to be the global leader in combating HIV/AIDS, we need to act like it," the president then said .
He also called the ban a "decision rooted in fear rather than fact."
The ban has kept out thousands of students, tourists and refugees and has complicated the adoption of children with HIV, immigration rights groups say. The United States has also been unable to host a major international AIDS conference because HIV-positive activists and researchers have been barred.
While immigration law still excludes foreigners with any "communicable disease of public health significance," HIV has been removed from the list of those meriting denied entry.
But some immigration control groups have been critical of the ban's repeal because of its potential cost to taxpayers.
Popular Reads

Woman found dead in her cubicle
- Aug 29, 7:16 PM

Stranded man was hiking for World Central Kitchen
- Aug 29, 11:51 AM
Arrest made in couple missing from nudist ranch
- Aug 30, 11:33 AM

Majority says Trump won't accept election: POLL
- Aug 30, 6:11 AM

Trump charged in Jan. 6 superseding indictment
- Aug 27, 6:25 PM
ABC News Live
24/7 coverage of breaking news and live events
- What Are HIV and AIDS?
- How Is HIV Transmitted?
- Who Is at Risk for HIV?
- Symptoms of HIV
- U.S. Statistics
- Impact on Racial and Ethnic Minorities
- Global Statistics
- HIV and AIDS Timeline
- In Memoriam
- Supporting Someone Living with HIV
- Standing Up to Stigma
- Getting Involved
- HIV Treatment as Prevention
- Pre-exposure Prophylaxis (PrEP)
- Post-exposure Prophylaxis (PEP)
- Preventing Sexual Transmission of HIV
- Alcohol and HIV Risk
- Substance Use and HIV Risk
- Preventing Perinatal Transmission of HIV
- HIV Vaccines
- Long-acting HIV Prevention Tools
- Microbicides
- Who Should Get Tested?
- HIV Testing Locations
- HIV Testing Overview
- Understanding Your HIV Test Results
- Living with HIV
- Talking About Your HIV Status
- Locate an HIV Care Provider
- Types of Providers
- Take Charge of Your Care
- What to Expect at Your First HIV Care Visit
- Making Care Work for You
- Seeing Your Health Care Provider
- HIV Lab Tests and Results
- Returning to Care
- HIV Treatment Overview
- Viral Suppression and Undetectable Viral Load
- Taking Your HIV Medicine as Prescribed
- Tips on Taking Your HIV Medicine as Prescribed
- Paying for HIV Care and Treatment
- Other Health Issues of Special Concern for People Living with HIV
- Alcohol and Drug Use
- Coronavirus (COVID-19) and People with HIV
- Hepatitis B & C
Vaccines and People with HIV
- Flu and People with HIV
- Mental Health
- Mpox and People with HIV
- Opportunistic Infections
- Sexually Transmitted Infections
- Syphilis and People with HIV
- HIV and Women's Health Issues
- Aging with HIV
- Emergencies and Disasters and HIV
- Employment and Health
- Exercise and Physical Activity
- Nutrition and People with HIV
- Housing and Health
- Traveling Outside the U.S.
- Civil Rights
- Workplace Rights
- Limits on Confidentiality
- National HIV/AIDS Strategy (2022-2025)
- Implementing the National HIV/AIDS Strategy
- Prior National HIV/AIDS Strategies (2010-2021)
- Key Strategies
- Priority Jurisdictions
- HHS Agencies Involved
- Learn More About EHE
- Ready, Set, PrEP
- Ready, Set, PrEP Pharmacies
- AHEAD: America’s HIV Epidemic Analysis Dashboard
- HIV Prevention Activities
- HIV Testing Activities
- HIV Care and Treatment Activities
- HIV Research Activities
- Activities Combating HIV Stigma and Discrimination
- The Affordable Care Act and HIV/AIDS
- HIV Care Continuum
- Syringe Services Programs
- Finding Federal Funding for HIV Programs
- Fund Activities
- The Fund in Action
- About PACHA
- Members & Staff
- Subcommittees
- Prior PACHA Meetings and Recommendations
- I Am a Work of Art Campaign
- Awareness Campaigns
- Global HIV/AIDS Overview
- U.S. Government Global HIV/AIDS Activities
- U.S. Government Global-Domestic Bidirectional HIV Work
- Global HIV/AIDS Organizations
- National Black HIV/AIDS Awareness Day February 7
- HIV Is Not A Crime Awareness Day February 28
- National Women and Girls HIV/AIDS Awareness Day March 10
- National Native HIV/AIDS Awareness Day March 20
- National Youth HIV & AIDS Awareness Day April 10
- HIV Vaccine Awareness Day May 18
- National Asian & Pacific Islander HIV/AIDS Awareness Day May 19
- HIV Long-Term Survivors Awareness Day June 5
- National HIV Testing Day June 27
- Zero HIV Stigma July 21
- Southern HIV/AIDS Awareness Day August 20
- National Faith HIV/AIDS Awareness Day August 25
- National African Immigrants and Refugee HIV/AIDS and Hepatitis Awareness Day September 9
- National HIV/AIDS and Aging Awareness Day September 18
- National Gay Men's HIV/AIDS Awareness Day September 27
- National Latinx AIDS Awareness Day October 15
- World AIDS Day December 1
- Event Planning Guide
- U.S. Conference on HIV/AIDS (USCHA)
- National Ryan White Conference on HIV Care & Treatment
- AIDS 2020 (23rd International AIDS Conference Virtual)
Want to stay abreast of changes in prevention, care, treatment or research or other public health arenas that affect our collective response to the HIV epidemic? Or are you new to this field?
HIV.gov curates learning opportunities for you, and the people you serve and collaborate with.
Stay up to date with the webinars, Twitter chats, conferences and more in this section.
- COVID-19 and People with HIV
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email

Should People with HIV Get Vaccines?
Yes. Vaccines play an important role in keeping people healthy. They protect you against serious and sometimes deadly diseases.
Vaccines are especially important for people with chronic health conditions like HIV, which can make it harder to fight off vaccine-preventable diseases like pneumococcal disease or the flu. HIV can also make it more likely that you’ll have serious complications from those diseases, which is why getting recommended vaccines is an important part of your overall HIV medical care.
Vaccines are very effective and they don’t just protect individuals from disease. They also protect communities. When most people in a community get vaccinated and become immune to a disease, there is little chance of a disease outbreak. Eventually, the disease becomes rare—and sometimes, it’s wiped out altogether.
COVID-19 Vaccines and People with HIV
Get vaccinated. CDC recommends everyone—including people with HIV—stay up to date with COVID-19 vaccines for their age group. According to CDC , here’s what you need to know:
- CDC recommends the 2023-2024 updated COVID-19 vaccines: Pfizer-BioNTech, Moderna, or Novavax, to protect against serious illness from COVID-19.
- Everyone aged 5 years and older should get 1 dose of an updated COVID-19 vaccine to protect against serious illness from COVID-19.*
- Children aged 6 months–5 years may need multiple doses of COVID-19 vaccine to be up to date , including at least 1 dose of updated COVID-19 vaccine.
- People who are moderately or severely immunocompromised (have a weakened immune system) may get additional doses of updated COVID-19 vaccine. This includes people with advanced or untreated HIV.
- People aged 65 years and older who received 1 dose of any updated 2023-2024 COVID-19 vaccine (Pfizer-BioNTech, Moderna or Novavax) should receive 1 additional dose of an updated COVID-19 vaccine at least 4 months after the previous updated dose. For more Novavax information, click or tap here.
- COVID-19 vaccine recommendations will be updated as needed.
- People who are up to date have lower risk of severe illness, hospitalization, and death from COVID-19 than people who are unvaccinated or who have not completed the doses recommended for them by CDC.
To learn more about CDC’s immunization recommendations for COVID-19 and other respiratory viruses, see CDC’s Respiratory Virus Guidance .
* People aged 12 years and older who have not previously gotten any COVID-19 vaccine doses and choose to get Novavax should get 2 doses of updated Novavax vaccine to be up to date .
What Are Vaccines?
Vaccines protect your body from diseases and infections such as COVID-19, human papillomavirus (HPV), influenza (flu), hepatitis B and polio. They are given by needle injection (a shot), by mouth, or sprayed into the nose.
Vaccines help your immune system fight infections faster and more effectively. When you get a vaccine, it sparks an immune response, helping your body fight off and remember the germ so it can attack it if the germ ever invades again. And since vaccines are made of very small amounts of weak or dead germs, they won’t make you sick.
Vaccines often provide long-lasting immunity to serious diseases without the risk of serious illness. Learn more about how vaccines work .
Which Vaccines are Recommended for People with HIV?
The following vaccines are recommended for people with HIV:
- Hepatitis A
- Hepatitis B
- HPV (for those up to age 26)
- Influenza (flu)
- Meningococcal series which protects against meningococcal disease
- Pneumococcal (pneumonia)
- Tetanus, diphtheria, and pertussis (whooping cough) . A single vaccine protects against the three diseases. Every 10 years, a repeat vaccine against tetanus and diphtheria (called Td) is also recommended
- Zoster (shingles) (for those ages ≥18)
Based on age or other circumstances, you provider may recommend other vaccines as well. Talk to your health care provider about which vaccines are recommended for you. For more details, see this chart from the Centers for Disease Control and Prevention (CDC.
Are All Types of Vaccines Safe for People Living with HIV?
Vaccines are generally safe for people with HIV. However, some types of vaccines may not be recommended. For example, live attenuated vaccines (LAV)—like the chickenpox vaccine —contain a weakened but live form of the germ that causes the disease. LAVs can potentially cause an infection for people with HIV. However, depending on age, health, previous vaccinations, or other factors, some LAVs may be recommended. Talk to your health care provider about what is recommended for you.
Can HIV Affect How Well a Vaccine Works?
Yes. HIV can weaken your body’s immune response to a vaccine, making the vaccine less effective. In general, vaccines work best when your CD4 count is above 200 copies/mm3.
Also, by stimulating your immune system, vaccines may cause your HIV viral load to increase temporarily.
Do Vaccines Cause Side Effects?
Any vaccine can cause side effects. Side effects from vaccines are generally minor (for example, soreness at the location of an injection or a low-grade fever) and go away within a few days.
Severe reactions to vaccines are rare. Before getting a vaccine, talk to your health care provider about the benefits and risks of the vaccine and possible side effects. Learn about vaccine safety and possible side effects.
What About Travel and Vaccines?
You should be up to date on routine vaccines, no matter where you are going. If you are planning a trip outside the United States, you may need to get vaccinated against diseases that are present in other parts of the world, such as cholera or yellow fever.
If you have HIV, talk to your health care provider about any vaccines you may need before you travel. He or she will know which ones are safe for you. Keep in mind: most travel vaccines can be given safely to people with HIV and others with weakened immune systems. However, they may be less effective than in people with strong immune systems, and may not provide full protection. Your doctor may recommend blood tests to confirm that a vaccine was effective, or recommend additional precautions to keep you safe.
Some travel vaccines are LAVs and many people with weakened immune systems should not take them. However, depending on the circumstances, the benefits of protection may outweigh the risks. Talk to your health care provider about what is recommended for you.
To learn more, see Traveling Outside the U.S.
Is There a Vaccine Against HIV?
No. There is currently no vaccine that has been approved by the FDA to prevent HIV infection or treat those who have it. However, scientists are working to develop both types. Learn about HIV vaccine research .
Related HIV.gov Blogs
Fyi video: a conversation about the importance of hiv vaccine research, oidp invites public comment on proposed viral hepatitis quality measures, nih research identifies opportunities to improve future hiv vaccine candidates.
- CDC – Flu and People Living with HIV
- CDC – Travelers with Weakened Immune Systems
- HIVinfo.NIH.gov – HIV and Immunizations
- HHS.gov/immunizations – Vaccine Basics
- HHS.gov/immunizations – Vaccines for People with Health Conditions

COMMENTS
Key points. A number of countries restrict the entry and/or residence of people with HIV. Tourism or business trips are generally possible, even in countries with entry bans. Long-term restrictions related to work or study permits are strictly enforced. Undetectability is never taken into account. Some countries limit entry for people with HIV.
View the U.S. State Department's information on insurance for overseas travel. Take proof of insurance, such as a photocopy or scan your policy and send the image to an e-mail address you can access both in the United States and abroad. Leave a copy at home and tell your friends or family where it is located.
Since January 4, 2010, people living with HIV can enter the U.S. like anybody else. Visitors under the visa waiver program (for countries where a visa is not required to travel to the USA) and are living with HIV: please note that HIV is no longer considered a communicable disease for entry purposes.
During travel to developing countries, people infected with HIV are at a much higher risk for food and waterborne disease than they are in the United States. Take extra precautions to avoid any uncooked foods, and make sure all water is either boiled or bottled. Traveler's diarrhea is a common problem. Carry a 3- to 7-day supply of medicine to ...
The rule restricting travel or immigration to the US by people living with HIV, often called the "HIV entry ban," was lifted in 2010 after 22 years by then-President Barack Obama. View our companion fact sheet, US Immigration and HIV: The Basics, for an overview of the US Immigration system. History of US Immigration, Health, and HIV
HIV infection occurs worldwide. In 2000, an estimated 37.7 million people were living with HIV infection globally. Sub-Saharan Africa is the most affected part of the world (25.4 million cases, or 67% of all people living with HIV infection); central Asia and eastern Europe have experienced the largest increases in new HIV infections (47% ...
Those with HIV, however, are more likely to get sick. Avoid hospitals and clinics where tuberculosis patients are treated. When you return home, ask your doctor if you should get tested for ...
A blunt instrument. Although one of the reasons for the US HIV ban is to control and monitor HIV-positive people entering the country, of the 135 who travelled to the US, only two (1,5%) actually travelled with an HIV waiver: 98,5% entered then country without the US knowing their HIV status.
The travel and immigration ban prohibited HIV-positive foreign nationals from entering the U.S. unless they obtained a special waiver, which was difficult to secure and then only allowed for short-term travel. The policy also prevented the vast majority of foreign nationals with HIV from obtaining legal permanent residency in the United States.
The countries or areas are sourced from the UN Statistics Division here The designations employed and the presentation of material do not imply the expression of any opinion whatsoever on the part of UNAIDS concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers ...
Ian Mackenzie / Flickr / CC BY 2.0. While efforts are being made to end similar laws throughout the world, the Global Database on HIV-Specific Travel & Residence Restrictions (a joint European initiative published by the International AIDS Society) reports that as of 2023, 56 out of 200 countries are known to have entry regulations for people living with HIV, and seven of these countries will ...
Thank-you for your question. There are no travel restrictions for HIV positive people traveling to the USA. All American travel restrictions relating to HIV status were lifted in January 2010. Customs regulations require people entering with prescription medication like antiretroviral drugs to carry a doctor's certificate in English, stating ...
HIV and Travel: 8 Tips Before You Go. Allow extra time. Check for restrictions. See your healthcare provider. Get vaccinated. Pack your medications. Keep medications close. Review your insurance ...
HIV-Positive Applicants Might Be Delayed Due to Enhanced TB Screening. The Centers for Disease Control (CDC) instructions to its civil surgeons (who perform medical exams for would-be immigrants) could delay, if not completely derail, some HIV-positive applicants' request for a visa to the United States. Tuberculosis screening requirements require that anyone known to be HIV positive undergo ...
Effective January 4, 2010, a diagnosis of HIV infection will not render a person traveling into the United States as inadmissible under Section 212(a)(1)(A)(i) of the Immigration and Nationality Act (INA). Thus, HIV-positive travelers seeking entry to the United States no longer need a waiver of inadmissibility to travel to the United States.This includes travelers who successfully obtained a ...
Traveling with HIV. Traveling outside the United States may require special precautions for people with HIV. For example, travel to some countries can increase the chances of getting an severe illness. Before you travel. Discuss medicine and vaccines with your health care provider at least 4 to 6 weeks before you travel.
On January 4, 2010, the HIV ban on travel and immigration, which had been in place for two decades finally came to an end. With the end of the HIV ban, being HIV positive is no longer an automatic ground of "inadmissibility." For foreign nationals seeking to enter as tourists or short-term visitors, being positive should not be an issue at all.
During travel to developing countries, people infected with HIV are at a much higher risk for food and waterborne disease than they are in the United States. Take extra precautions to avoid any uncooked foods and make sure all water is either boiled or bottled. Traveler's diarrhea is a common problem. Carry a three- to seven-day supply of ...
Since my own HIV diagnosis in 2001, as a self-employed writer, I'd received my health care via New York state's comparatively excellent ADAP program—which paid the full premium and copays on ...
According to HIV Travel, there are currently a total of 12 world countries that keep restrictions for short-term stays (under 90 days) in place for people living with HIV. The full list of countries with visa restrictions for short-term stays for people with HIV is as follows: Bhutan. Brunei. Egypt.
WASHINGTON, Jan. 5, 2010— -- In a move public health and human rights advocates have hailed as a "victory," the so-called HIV travel ban, which barred entry to the U.S. by people living with ...
CDC recommends everyone—including people with HIV—stay up to date with COVID-19 vaccines for their age group. According to CDC, here's what you need to know: CDC recommends the 2023-2024 updated COVID-19 vaccines: Pfizer-BioNTech, Moderna, or Novavax, to protect against serious illness from COVID-19. Everyone aged 5 years and older should ...
Are you planning to travel outside the United States? Visit the Centers for Disease Control and Prevention's (CDC) website at wwwnc.cdc.gov/travel/ ... Adults with HIV infection need to get either PCV20 alone, or PCV15 followed at least 8 weeks later by PPSV23. If you have previously received either PCV13 and/or PPSV23, your healthcare ...